|
As my career has advanced I have found my own little niches that I am drawn to, "caring for the caregiver" is one. For those that are caregivers to their parents, children, spouse, or siblings, it is often the caring for their own self that is forgotten. Caring for themselves is one of the most important, one of the most often forgotten things they can do as a caregiver. In fact, when their needs are taken care of, the person they are caring for will benefit too. I would like to take the time to share a few tips, signs of burnout, and services available to caregivers. Many times, attitudes and beliefs form personal barriers that stand in the way of caring for yourself. Identifying personal barriers: • Do you think you are being selfish if you put your needs first? • Is it frightening to think of your own needs? What is the fear about? • Do you have trouble asking for what you need? Do you feel inadequate if you ask for help? • Do you feel you have to prove that you are worthy of the care recipient's affection? Do you do too much as a result?  Identifying signs of burnout: • Physical : Feeling tired most of the day Feeling sick a lot Change in appetite or sleep Frequent headaches, back pain, muscle aches • Emotional: Sense of failure or self-doubt Feeling helpless, trapped Loss of motivation Having a negative outlook • Behavioral: Withdrawing and isolating Procrastinating Using food or alcohol to cope Taking frustrations out of others
0 Comments
 As I transition into my 2nd year blogging, I have decided to welcome in guest bloggers. I feel there are so many wonderful experiences out there that only benefit others if they are told. As I said before, this blog is here to "help us determine different learning experiences". Hope you all enjoy Sarah from OT Potential, if you haven't checked out her page you should! LIVE LIKE YOU ARE LEAVING... I am excited to be serving as a guest blogger on OT Huddle. I love the sharing that is happening here and hope to see more from “m.” A theme of the past few posts on OT Huddle has been transitions. I myself am a relatively new therapist and am starting to realize how common of an experience it is for young therapists to transition between several jobs, as we seek to find where our skill set and interests best intersect, in addition to figuring out where our jobs fit with relationships, babies, etc. I recently concluded time at a job that I loved. My reason for leaving was that our family is moving, not that I was unsatisfied with the work place. My last couple months there were just glorious. I felt like I was able to do the kind of work for which I went to OT school. I felt close to my team. I was on board with the overall mission. I was learning new things. I felt like I was making a difference. Basically, I was on OT cloud nine. Part of feeling was definitely that the setting was a good fit for me. But, part of how I experienced the past couple months was definitely attitudinal. I had an end date in mind. This did three things... As I celebrate my 2nd wedding anniversary and my 1st anniversary of being in the blog world, I am able to reflect on all the changes life has brought to me. Though great changes, they left me not blogging as often as I would love. In my second year I would love for that to change and my goal is to share the field I love more and more. I'll begin by sharing one of the many exciting opportunities I've had this past year.
For those who know me, I often make the joke about how much "I love butts"; well, working on a spinal cord unit allows my love for butts to blossom into full fruition. Throughout the last 6 months I have had the opportunity to work with, and learn, from several wound certified clinicians. Pressure sores ("bed sores"), moisture associated wounds, and wounds from friction and sheer are unfortunately not lacking among my population; I have been lucky enough to take part in helping manage and prevent these wounds during my work week. I've also had the opportunity to brainstorm and create some awesome custom cushions... with that I mean, COMMODE CUSHIONS! Take a look...  Some may think transitions are difficult, others take them on as a challenge. Maybe it is the actual transition...we go through so many each and every year, some small and some monumental. You would think at some point in our lives we would get used to change and get better at managing it, but will we ever? Perhaps our anxiety is the fear of unknown, the fear of losing control, change...letting go can be frightening. However, maybe we need to start looking at it as something good, a time to give us unique view on personal growth...a new beginning, a time for opportunity! I have been absent for some time secondary to going through transitions in my life. Changing the OT setting that I work in is one transition. With that I found myself lost, wondering where I fit into the blog world. A good friend reminded me about simplicity, "blog about your transition", she said. 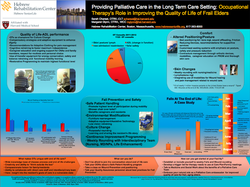 I am lucky enough to work with an amazing group of therapists, two of whom I was able to learn the ins and outs of the long term care (LTC) unit from. Sarah Charest, OTR/L-CLT and Margaret Glynn, OTR/L-WCC had the opportunity to share their passion and expertise at the AOTA conference this year discussing "Occupational Therapy’s Role in Improving the Quality of Life of Frail Elders". I would love to take the time to share the work that they shared with us during our Huddle. What makes OTs unique with end of life care?
 ...if we learn most from our mistakes. I am a very new OT out in the field, to be exact 496 days (aka 1 yr and 18.85 wks). I still go into treatment sessions with a mixture of nervousness and excitement. Nervous that I won't find the "just right" activity for my patient and create a session where I feel guilty as if I wasted their time and I did not benefit the patient to the best of my ability. Excited that I WILL “hit the nail of the head” and have an awesome session that continues to build a rapport with my patient. We all make mistakes, have difficult sessions, or misinterpret what we think will be best, but hopefully we learn from them and they help us grew into a better therapist. I often think about the first big whoops I made as an OT, one that happened only a few hours into my first job; in fact, one that happened with the first patient I treated on my own as an OTR/L.  Let me begin by telling you a bit about the facility I work in. It is a sub-acute facility; sometimes we see patients typical for a SNF (skilled nursing facility) however we are fortunately enough to have LTAC (long-term acute care) the floor above us, so occasionally those individuals will transfer down to our floor making us sub-acute. In any case, our facility is made of two large buildings, the building attached to our rehab housing LTC (long-term care) residents as well as the facilities' gift shop, synagogue/chapel, laundry machines, our beloved ramp. :) The distance from the rehab to the gift shop, etc. would be "community mobility" ie- 150' x4. I feel that we are VERY LUCKY in how creative we can get with activities, especially those for "higher-level" patients, however we always can be motivated by new ideas. Our huddle a couple weeks ago discussed a variety of standing activities to use that are more "grown up" - rather than putting a brightly colored ring arch in front of them. (don't get me wrong I do love my ring arch). Here is what we discussed... 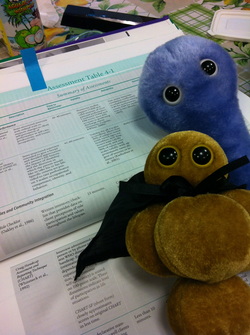 First and foremost, as you can see in the picture, MRSA and C-Diff (the stuffed animals of course) joined us for our first huddle. I'm sure they will pop in and out occasionally! Our initial HUDDLE was taken over by the fact that Medicare has yet again changed guidelines for billing. Surprised? On our unit we maybe get a Med B patient once everyone couples months, but we felt it necessary to review what these new guidelines were and possible assessment tools that they be beneficial to add to our OT department. According to AOTA, as of July 1st CMS is requiring functional report for all OT reimbursement. Therefore, a therapist must choose a patient's primary functional limitation to report a G-code and modifier on. The functional areas in which OTs work on are the following: mobility, changing and maintaining body position, attention, memory, carrying/moving/handling objects, etc. Once a primary G-Code has been chosen for a particular limitation, a modifier that reflects a patient's score/severity on a particular functional assessment tool should be identified. AOTA provides a link to a great website that provides conversions for G-Codes and a search engine for assessment tools. HELLO to fellow OTs!
I have been wanting to create a group for the OTs of my sub-acute rehab unit to further our knowledge and experiences between each other. After much deliberation (and a couple of Dark & Stormies), a friend and I brainstormed the group name to be HUDDLE …
Most therapists typically participate in journal club groups, but how many people have time/energy to read journals after going to yoga, or putting the kids down, or taking the pup for a walk?! I thought our unit would benefit from having a group where we can all bring some of the following to the group to discuss, brainstorm, and possibly learn from. Here I am to share it with you as well. Here is what we discuss:
I hope this group be a great way to share the experiences we have in our field so we can all benefit and learn for our future patients we may have the opportunity to treat hands on. I also hope whomever may come across this in their google searches will learn and enjoy as well. I would love to hear about every OT's experiences and maybe I can share them here as well. ENJOY this leisure activity! Functionally yours, m |

 RSS Feed
RSS Feed
